MPOX
MPOX is a viral infection that can cause a painful rash, enlarged lymph nodes, fever and infectious lesions. It is spread through close skin-to-skin physical contact with someone who has symptoms. Most people fully recover, but some get very sick.
Vaccination against MPOX is available in New Zealand for those most at risk, please contact your local Sexual Health Clinic for details, or if you are in Auckland, call Auckland Sexual Health on 0800 739432.
MPOX Vaccine in New Zealand
A vaccine for people at risk of MPOX is available if prescribed by a medical practitioner to people who meet the eligibility criteria. Those eligible for the vaccine include:
- Close physical contacts of people infected with MPOX, such as sexual partners and people who live in the same household.
- Gay, bisexual and other men who have sex with men (GBMSM) who have multiple sexual partners, and trans and cisgender women who are in intimate relationships with these eligible men.
- Those recommended to have the vaccine by medical specialists.
- For an initial assessment to check if you are at risk of MPOX and eligible for the vaccine, please contact your local Sexual Health Clinic or if you are in Auckland, call Auckland Sexual Health on 0800 739432.
- People who are not NZ residents (including international students, seasonal workers and visitors) will also be able to access MPOX consultation and testing free of charge.
Why is the MPOX Vaccine not being promoted more openly in NZ?
The vaccine can only be made available under section 29 of the Medicines Act 1981. This allows for ‘unapproved’ vaccines to be provided to individual medical practitioners for a particular patient after assessing the patient’s needs. The Act also prevents the brand name of the vaccine being promoted due to its ‘unapproved’ status.
Advertising the availability of unapproved medicines is prohibited by section 20 of the Medicines Act 1981. This means that the vaccine cannot be advertised, nor its availability promoted. It can only be offered by a medical practitioner to a consumer as a proposed medical treatment and then administered after a full informed consent process.
The vaccine can only be made available under section 29 of the Medicines Act 1981. This allows for ‘unapproved’ vaccines to be provided to individual medical practitioners for a particular patient after assessing the patient’s needs. The Act also prevents the brand name of the vaccine being promoted due to its ‘unapproved’ status.
Advertising the availability of unapproved medicines is prohibited by section 20 of the Medicines Act 1981. This means that the vaccine cannot be advertised, nor its availability promoted. It can only be offered by a medical practitioner to a consumer as a proposed medical treatment and then administered after a full informed consent process.
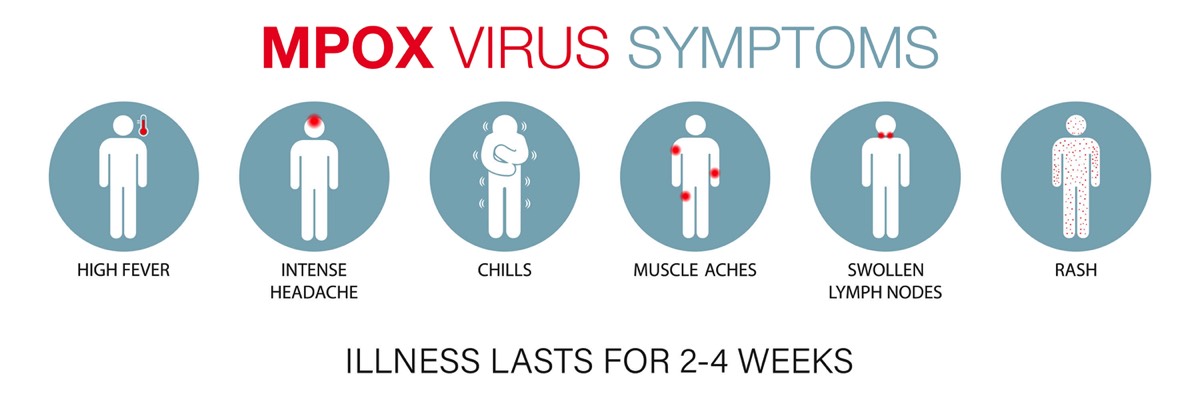
What are the symptoms?
The mean incubation time is 7 days with initial symptoms of a flu-like illness with fever, malaise, headache, and fatigue often accompanied by swelling of lymph nodes.
Shortly after a rash can appear with lesions before scabbing. The lesions are the infectious component and usually occur at the site of contact eg throat/mouth for receptive oral sex. Most persons have fewer than 10 lesions and almost 10% present with only a single genital lesion. Hospitalisation is uncommon and the major reason for admission is usually for pain control, typically for anorectal or oral pain. Complications can occur if there is a secondary infection of the lesion. The symptoms usually resolve by themselves within a few weeks, but you are considered infectious while you have symptoms.
Shortly after a rash can appear with lesions before scabbing. The lesions are the infectious component and usually occur at the site of contact eg throat/mouth for receptive oral sex. Most persons have fewer than 10 lesions and almost 10% present with only a single genital lesion. Hospitalisation is uncommon and the major reason for admission is usually for pain control, typically for anorectal or oral pain. Complications can occur if there is a secondary infection of the lesion. The symptoms usually resolve by themselves within a few weeks, but you are considered infectious while you have symptoms.
If you think you may have symptoms, you should isolate and seek medical advice from your primary care physician, sexual health clinic or contact Healthline on 0800-611-116. You may be asked to isolate until test results are returned.
Probable and confirmed cases will need to isolate for a minimum of 7 days from the first presence of lesions, and then take other precautions to prevent onward transmission once released from isolation. They must continue taking precautions until they are no longer infectious which is until their lesions have crusted, the scab has fallen off and a fresh layer of skin has formed underneath (symptoms normally last 14–28 days). There is no specific financial support available at this time.
Probable and confirmed cases will need to isolate for a minimum of 7 days from the first presence of lesions, and then take other precautions to prevent onward transmission once released from isolation. They must continue taking precautions until they are no longer infectious which is until their lesions have crusted, the scab has fallen off and a fresh layer of skin has formed underneath (symptoms normally last 14–28 days). There is no specific financial support available at this time.
How is it transmitted?
MPOX is transmitted through intimate skin-to-skin contact with the skin lesions. Contaminated objects such as bedding, clothing, or sex toys can also carry the virus but have much lower risk.
It is not classified as a sexually transmitted infection, but sex can make its transmission easy and is considered to be a common driver of transmission in the current outbreaks.
A recent study (The Lancet), found that MPOX transmits most efficiently when lesions come into contact with mucus membranes in the anus, rectum, genitals, mouth and throat. MPOX is more likely to transmit through oral or anal sex than through contact with external skin, which would need some sort of defect, such as a wound, to allow entry of the virus.
It is not classified as a sexually transmitted infection, but sex can make its transmission easy and is considered to be a common driver of transmission in the current outbreaks.
A recent study (The Lancet), found that MPOX transmits most efficiently when lesions come into contact with mucus membranes in the anus, rectum, genitals, mouth and throat. MPOX is more likely to transmit through oral or anal sex than through contact with external skin, which would need some sort of defect, such as a wound, to allow entry of the virus.
MPOX & HIV
People with advanced HIV infection or who are not taking antiretroviral drugs might be at increased risk for severe disease if they get MPOX.
However there does not appear to be more severe MPOX illness in people who have HIV, are on antiretroviral medication and are virally suppressed.
However there does not appear to be more severe MPOX illness in people who have HIV, are on antiretroviral medication and are virally suppressed.
What treatment is available?
For most patients, treatment for MPOX is mainly supportive, such as pain medication. Most people with MPOX recover fully within 2 to 4 weeks without the need for medical treatment.
There are no treatments specifically for MPOX virus infections. However, MPOX and smallpox viruses are genetically similar, which means that antiviral drugs and vaccines developed to protect against smallpox may be used to prevent and treat MPOX virus infections. New Zealand has secured 504 doses of Tecovirimat, also called Tpoxx which is reserved for severe cases who need to be hospitalised.
Tecovirimat is an antiviral medication approved by the FDA for treatment of smallpox in adults and children but not for MPOX because data are not available on the effectiveness of Tecovirimat in treating MPOX in humans.
There are no treatments specifically for MPOX virus infections. However, MPOX and smallpox viruses are genetically similar, which means that antiviral drugs and vaccines developed to protect against smallpox may be used to prevent and treat MPOX virus infections. New Zealand has secured 504 doses of Tecovirimat, also called Tpoxx which is reserved for severe cases who need to be hospitalised.
Tecovirimat is an antiviral medication approved by the FDA for treatment of smallpox in adults and children but not for MPOX because data are not available on the effectiveness of Tecovirimat in treating MPOX in humans.
Studies using a variety of animal species have shown that Tecovirimat is effective in treating orthopoxvirus-induced disease. Human clinical trials indicated the drug was safe and tolerable with only minor side effects. A case report from the UK suggested that Tecovirimat may shorten the duration of illness and viral shedding.
Is there a vaccine for MPOX?
The Jynneos vaccine is a 2 dose vaccine that is being used for MPOX. This requires two shots 4 weeks apart with maximum effectiveness attained 2 weeks after the second shot. Jynneos has been specifically evaluated in people with HIV and shown to be safe.
If you have been vaccinated for smallpox in the past this shows limited protection as the efficacy wanes over time and cases have still occurred. Research from the Spanish outbreak showed 18% of cases were amongst people that had previously been vaccinated as children.
If you have been vaccinated for smallpox in the past this shows limited protection as the efficacy wanes over time and cases have still occurred. Research from the Spanish outbreak showed 18% of cases were amongst people that had previously been vaccinated as children.
If you are in Auckland and would like to be offered the vaccine, call Auckland Sexual Health on 0800 739432 for an appointment, otherwise please contact your local Sexual Health Clinic for details on what is available in your area.
Join Body Positive
By becoming a member you will be able to access all the services we offer, as well as support and updates to help you live better.
Newsletter
Want to be keep up with whats happening at Body Positive?
Subscribe to our newsletter below by submitting your e-mail address.
Subscribe to our newsletter below by submitting your e-mail address.